What I See as Your Pain Points
WHY?


WHY?

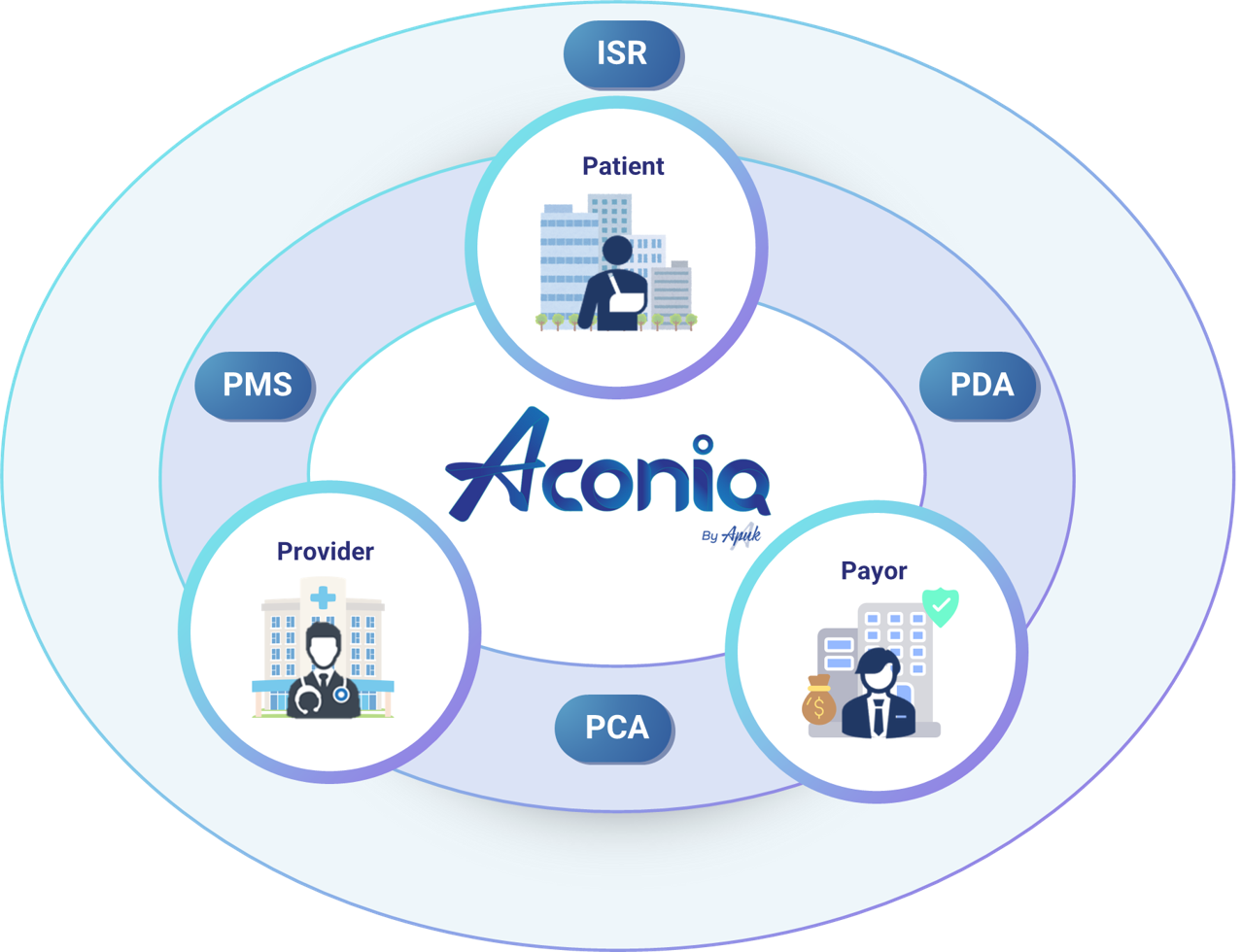
Who Can Help Minimize the Causes of Your Pain Points
You need a partner who can …
… and that partner is …


From insurers to consumers, we build technology that makes insurance work smarter, faster, and fairer.
Aconiq by APUK is an AI-assisted solution that enhances understanding and alignment across the claim journey for patients, providers, and payors.
It delivers real-time insights into medical and insurance facts, guides patients to preferred providers, and ensures clear communication before treatment. This fosters realistic expectations and greater satisfaction.
Financially, it helps patients minimize out-of-pocket costs, reduces bad debt risks for providers, and prevents claim leakage and reputation loss for payors.